UX Design - AI Health Web Application
OpenRoom
Utilizing the power of AI to automate and streamline the hospital discharge form generation.
Project Overview
Problem
Hospitals lose time and money to discharge delays. Hospital discharges take up to 2.2 hours per patient and on average discharge summaries consume 135 hours a week for the medical workforce.
Delays in completing hospital discharge summaries have also been linked to a greater risk of patients returning to hospital within 30 days — as each day’s delay in finalising a summary was associated with a 1.6% increased chance of readmission.
Approach
Carried out literary review to assess problem to solve
Led research interviews; synthesised findings
Ran ideation workshops
Created functioning prototype as a team
Solution
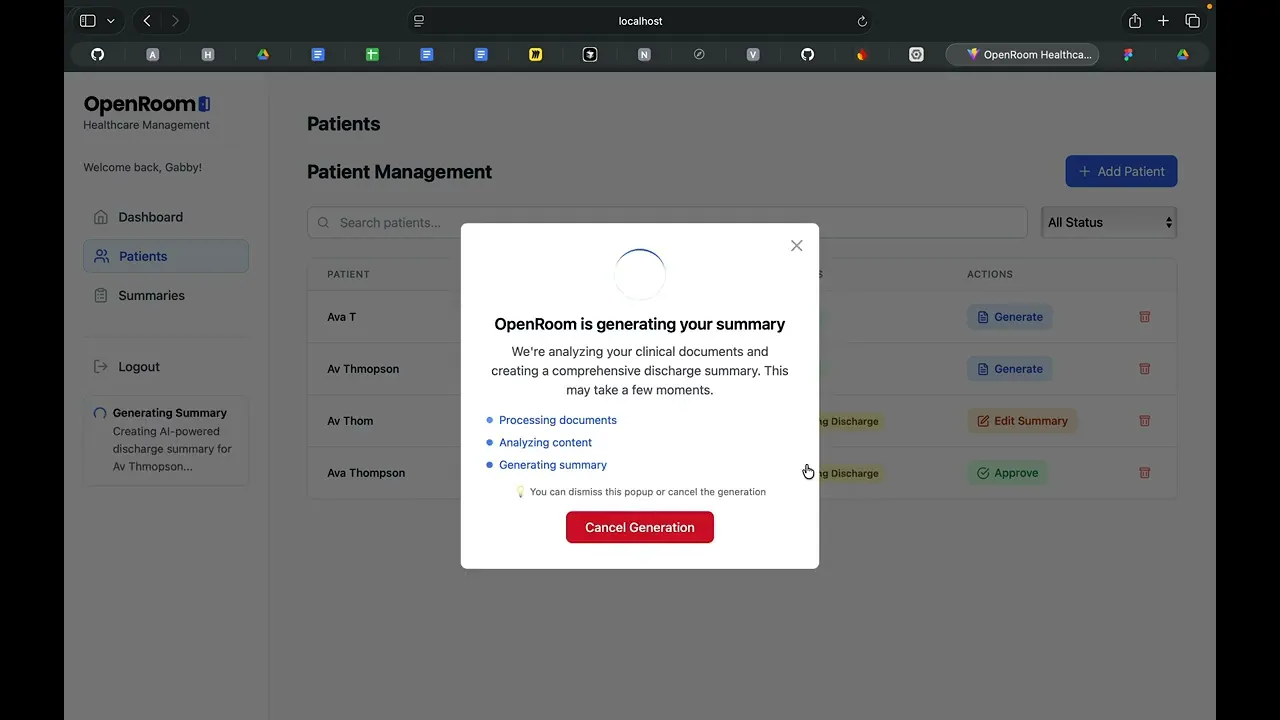
We designed OpenRoom, an AI system that extracts medical notes, generates accurate draft summaries and updates bed managers in real time.
Outcome
A fully tested prototype ready for implementation where 90% of clinicians were satisfied with the clarity and usability.
Role
UX Designer / Researcher
Team
Gabrielle Versace
Pragrun Ramesha
Pete Argent
Emannuelle Berkowicz
Tools
Miro
Figma
Bolt AI
Define
I ran a collaborative workshop with the team consisting of our UI designer and AI developers to bring the team to a unified consensus of the problem space and brainstorm solutions that were viable for the AI developers of our team to implement and understand the 'why'.
We utilised a pre-existing discharge summary template and referred to a real-life example of a discharge summary from a group member who had been in hospital to understand how it had been used on the patient side.
Discovery
Research Goals
Through our research we wanted to:
Understand how discharge summaries are currently written (tools, workflows, pain points).
Validate if OCR + NLP automation could reduce effort and backlog.
Test whether clinicians trust/edit AI-generated discharge drafts.
Identify what would make an AI-assisted discharge tool adoptable in a high-pressure hospital setting.
We used two research methods to do this: secondary research through a review of academic literature, and primary research through user interviews.
Literature Review
Our team began the design process by contextualising the issue through academic sources such as RACP Internal Medicine Journal, The Open Orthopaedics Journal and The Limbic which gave a good overview of the problems that medical practitioners face.
Findings included:
Writing a discharge summary took a median of 14.5 minutes, with almost six minutes of that spent on “thinking time” or searching for information rather than typing.
The patient discharge process was delayed at three points: discharge summary dictation by primary care team, transcription of summary and authentication of dictation by primary care physician.
Possible causes of discharge summary delays cited the burden of manual data entry, limited EMR usability, competing clinical demands, lack of standardisation and inadequate TMO engagement, including during handovers.
User Interviews
I led 1hr semi-structured interviews with potential users and people familiar with the issue:
Senior Doctor
Junior Intern Doctor
Radiologist
Key findings included:
Searching for the relevant information in the clinical notes takes most of the time.
Lack of planning in the preparation of the discharge summary— afterthought rather than a planned process.
The discharge summary is often given to junior doctors who have not treated the patient. Which causes extra time because the [junior] doctor needs to review and learn the entire patient history to summarise it which is timely.
The senior doctor then takes over the discharge summary but has no ownership over it. "It's chaotic."
A draft which needs to be edited by the clinician, would only work well if the person using it is the treating doctor (which is what should be happening). Doctors feels that the treating doctor should be [handling discharge summary].
Implementation
Watch the demo video ↓















